What Is the Normal Range for Blood Test Cholesterol? A Quick Guide
When your doctor hands you a lab report, the dreaded line “Total Cholesterol: 190 mg/dL” can feel like a cryptic crossword clue. But understanding the normal range for blood test cholesterol is as simple as decoding a recipe: it tells you whether your body’s “fuel” is in the sweet spot or if you’re cooking up a storm of risk. In this article we’ll break down the numbers, explain why they matter, and give you a cheat sheet to keep your cholesterol in check—without turning your kitchen into a science lab.
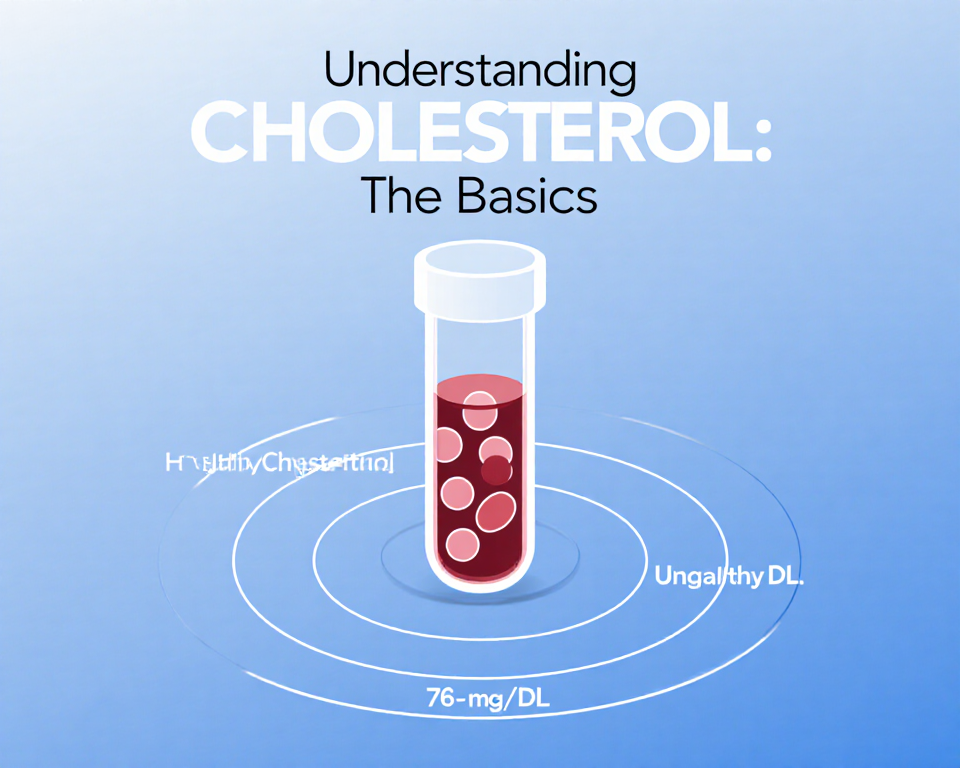
Understanding Cholesterol: The Basics
Types of Cholesterol
Cholesterol travels in the bloodstream on lipoprotein carriers. Think of them as delivery trucks:
- LDL (Low‑Density Lipoprotein) – the “bad” truck that can clog arteries.
- HDL (High‑Density Lipoprotein) – the “good” truck that ferries cholesterol back to the liver for disposal.
- VLDL (Very Low‑Density Lipoprotein) – carries triglycerides, another fat that can build up in vessels.
Why It Matters
High cholesterol is often called the “silent thief” because it can quietly damage arteries before you notice symptoms. Imagine a highway where traffic jams form over time—eventually, the flow breaks down. Cholesterol levels help predict the likelihood of heart disease, stroke, and other vascular problems.
The Normal Ranges Explained
Total Cholesterol
- Desirable: < 200 mg/dL
- Borderline high: 200–239 mg/dL
- High: ≥ 240 mg/dL
A total below 200 mg/dL is usually considered safe, but it’s only the headline. The story is in the details.
LDL (Low‑Density Lipoprotein)
- Optimal: < 100 mg/dL (or < 70 mg/dL for high‑risk individuals)
- Near optimal: 100–129 mg/dL
- Borderline high: 130–159 mg/dL
- High: 160–189 mg/dL
- Very high: ≥ 190 mg/dL
LDL is the villain in most cardiovascular narratives. Lower numbers mean fewer “roadblocks” in your arteries.
HDL (High‑Density Lipoprotein)
- Low (risk factor): < 40 mg/dL for men, < 50 mg/dL for women
- Normal: 40–59 mg/dL
- High (protective): ≥ 60 mg/dL
HDL is the “clean‑up crew.” The higher, the better—though a ridiculously high HDL may have its own quirks.
Triglycerides
- Normal: < 150 mg/dL
- Borderline high: 150–199 mg/dL
- High: 200–499 mg/dL
- Very high: ≥ 500 mg/dL
Triglycerides are the energy reserve; when they pile up, they can contribute to plaque formation.
Factors That Shift the Numbers
Diet
- Saturated fats (e.g., butter, cheese) raise LDL.
- Trans fats (fried foods, baked goods) spike LDL and lower HDL.
- Fiber (oats, beans) helps lower LDL.
- Omega‑3 fatty acids (salmon, walnuts) boost HDL.
Exercise
Regular aerobic activity can lift HDL by 5–10 mg/dL and lower triglycerides. Even a brisk 30‑minute walk can make a difference.
Genetics
Familial hypercholesterolemia is a genetic condition that can push LDL into the 300–400 mg/dL range. It’s the “genetic elevator” that bypasses lifestyle.
Age & Gender
Men generally have higher LDL earlier in life, while women’s LDL rises after menopause. HDL tends to be higher in women pre‑menopause.
Interpreting Your Results
How to Read the Lab Report
- Total Cholesterol: Gives a snapshot but hides the subtypes.
- LDL & HDL: Show the “good” vs “bad” balance.
- Triglycerides: Check for metabolic issues.
If your LDL is 140 mg/dL and your HDL is 45 mg/dL, you’re in a borderline high LDL territory but still within normal HDL. That’s a subtle warning sign.
When to Seek a Doctor
- LDL ≥ 190 mg/dL: Immediate medical review.
- Total Cholesterol ≥ 240 mg/dL: Discuss lifestyle changes or medication.
- Triglerycides ≥ 200 mg/dL: Evaluate for metabolic syndrome.
Remember, numbers are guidelines, not gospel. Your overall risk profile—including family history, smoking status, and blood pressure—matters just as much.
Managing Your Cholesterol
Lifestyle Tweaks
- Swap butter for olive oil in cooking.
- Add a handful of nuts daily for healthy fats.
- Incorporate leafy greens for soluble fiber.
- Aim for 150 minutes of moderate exercise per week.
Medications
If lifestyle changes aren’t enough, doctors may prescribe:
- Statins (e.g., atorvastatin) to lower LDL.
- PCSK9 inhibitors for high‑risk patients.
- Fibrates to reduce triglycerides.
Always discuss potential side effects and monitor liver enzymes if on statins.
Quick Tips & Checklist
- Check your numbers annually or as recommended by your healthcare provider.
- Track your diet with a food diary; look for hidden trans fats.
- Set a weekly exercise goal—even a 20‑minute walk counts.
- Stay hydrated; water helps flush excess lipids.
- Review medication side effects with your doctor.
Putting the Pieces Together
Cholesterol is like a traffic system: a few cars (LDL) can cause congestion, but a smooth flow (HDL) keeps everything moving. By understanding the normal range for blood test cholesterol, you can spot when your body’s traffic is getting jammed and take action before a heart‑breakingly bad incident occurs.
The next time you glance at a lab report, remember that the numbers are just a snapshot—your lifestyle is the engine that determines how long that snapshot lasts. Keep the fuel clean, the roads clear, and your heart will thank you.
If you’re ready to take the wheel, schedule a check‑up or update your diet plan today. Your future self will applaud you for the proactive steps you took now.